Do You Really Need a Pelvic Exam?
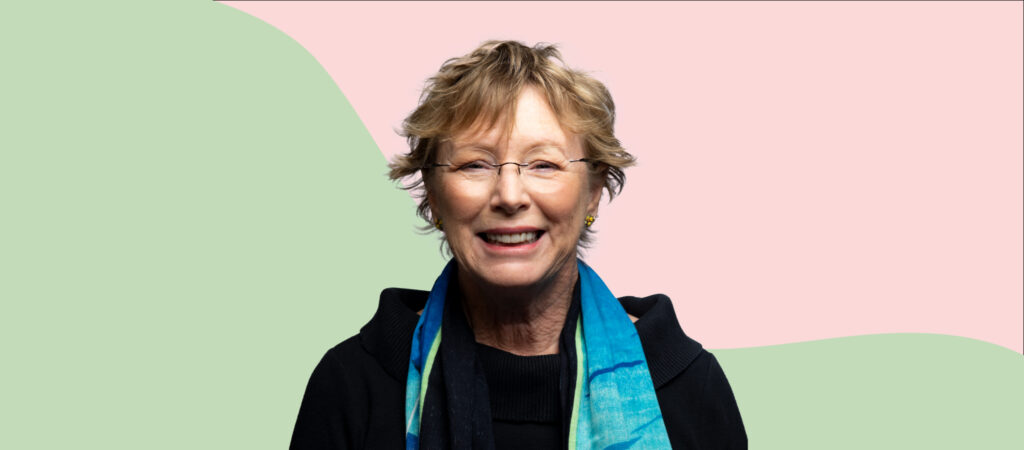
Our Dr. Julie Graves weighs in on disturbing news about unneeded pelvic exams, and explains when you do (and don't) need to undress from the waist down.
Women, how old were you when you first put your feet into metal stirrups so a doctor could perform a pelvic exam? If you were younger than 21 then the uncomfortable, possibly painful, probing you experienced likely wasn’t necessary.
In the past doctors believed that a pelvic exam was needed every year once periods started, and definitely once a woman started having sex. But over the past few decades, evidence has made clear that routine pelvic exams for women younger than 21 are unnecessary — so I was nothing short of outraged when I read the recent study finding that an estimated 1.4 million teen girls and young women in the U.S. received unnecessary pelvic exams between 2011 and 2017.
Let’s face it, pelvic exams aren’t fun at any age, and minors are likely to feel especially vulnerable with their feet in the stirrups — just think of the power gulf between a teen girl and the adult doctor performing the exam. Pelvic exams can be nothing short of traumatic for some women, especially those who have been victims of sexual assault in the past.
Even worse, some pelvic “exams” are a sexual assault. Predatory doctors abusing their patients this way have made headlines over the past few years because of USA Gymnastics doctor Larry Nassar and USC campus gynecologist Dr. George Tyndall, and again in January when Evelyn Yang spoke out about her abuse at the hands of an obstetrician. We all know there are similar sexual assaults that don’t make headlines, either because women don’t feel empowered to speak up or because their voices are silenced.
When Do You Need a Pelvic Exam?
Make no mistake, I’m not anti-pelvic exam, just against unnecessary ones. There are two very good reasons a woman should receive a pelvic exam: One, because she’s experiencing symptoms — such as abnormal bleeding, pain, or especially difficult periods — that need to be checked out. Or, two, for routine screening for precancerous changes that could lead to cervical cancer. Because these precancerous changes don’t cause noticeable symptoms, screening is needed to catch them before they turn cancerous.
For women without symptoms or risk factors, routine pelvic exams and Pap tests should begin starting at age 21, and no sooner. After age 21, they’re recommended every three years until age 30, and after 30 women have the option of getting an HPV test without a pelvic exam if they choose. So says the U.S. Preventive Services Task Force, the highly-esteemed group of clinicians and researchers who rigorously examine evidence to make recommendations for preventive care. These recommendations are designed to provide optimal prevention while following the physician’s mandate to “do no harm.” Beyond women and girls’ experiences during the exams themselves, unnecessary pelvic exams can cause harm in the form of false positives and follow-up testing, which can be scary, inconvenient, and expensive.
The reason for routine pelvic exams and Pap tests are unnecessary before age 21 is that cervical cancer is extremely rare in young women, and develops slowly at any age. Even if a girl starts sexual activity in her early teens and catches a dangerous strain of HPV (the sexually transmitted virus that causes the majority of cervical cancer), a first Pap test at 21 will protect her, because her body is likely to have cleared the virus on its own, and cervical cancer takes years to develop in any case. And assuming she has received the HPV vaccine (recommended for all girls and boys in their preteens) the already low risk of cervical cancer in this age group becomes practically nonexistent.
A sexually active teenager should be tested for sexually transmitted infections, and receive counseling from a provider on her birth control options, but neither of these necessarily requires a pelvic exam. Of course, if a teenage girl, or woman of any age, experiences worrisome symptoms, like very painful or heavy periods, inability to insert a tampon, or any symptom that causes her concern, then she should have a pelvic exam to help understand the source of the symptoms, and rule out conditions such as endometriosis.
Why Do Doctors Perform Unnecessary Pelvic Exams?
The USPSTF updated its screening recommendations for women under 21 in 2012, so why were doctors still giving teens pelvic exams in 2017? And teens aren’t the only ones undergoing unnecessary exams — many adult women still receive Pap tests annually despite the recommendations of the USPSTF that every 3-5 years is plenty for women without symptoms or risk factors.
I’m sure that the majority of doctors performing unneeded exams do so out of ignorance of the USPSTF recommendations, or because this is just the way they’ve “always done things.” But that’s no excuse for continuing a practice that may cause harm. Doctors should provide care that is based on evidence, not work on autopilot according to what they learned years ago in medical school.
As a doctor who has educated medical students and residents over the years, I hope that this study serves as a reminder to the medical community to stay up to date and treat our patients with the evidence-backed care they deserve. I emphasize that healthcare providers should be life-long learners, and remember that the standard of care they were trained in will evolve over time. I’m angry that so many doctors were not following the current guidelines about pelvic exams — our patients deserve better. I hope that this study opens a lot of eyes and leads physicians to change how they practice.
I also hope that patients who read this have the courage to say no to unnecessary tests. Ask questions about whether and why a test is required, and go to evidence-based sources of information, like the CDC website and US Preventive Services Task Force. I love it when my patients come in with information about their medical history and that of their family members, their symptoms, their questions, and what they’ve been reading, so we can have a thorough discussion about what is best for them. All healthcare providers should listen to their patients, provide evidence-backed information, and offer shared decision-making. If you feel like your questions aren’t answered, and your concerns aren’t heard, you can and should find another doctor.
About the Author
Dr. Julie Graves is a family medicine and public health doctor, as well as the Associate Director of Clinical Services at Nurx. She has more than 20 years of experience and has practiced medicine in Texas, Florida, Maryland, Wisconsin, Washington, DC, Sint Maarten, Germany, and even on a cruise ship. Dr. Graves also enjoys working in telehealth because it provides patients with convenience and comfort, enables them to ask questions at any time, and protects their privacy.
This blog provides information about telemedicine, health and related subjects. The blog content and any linked materials herein are not intended to be, and should not be construed as a substitute for, medical or healthcare advice, diagnosis or treatment. Any reader or person with a medical concern should consult with an appropriately-licensed physician or other healthcare provider. This blog is provided purely for informational purposes. The views expressed herein are not sponsored by and do not represent the opinions of Nurx™.